KSMO 2025
AI-powered Cell Type Quantification from Pre-neoadjuvant Slides as a Biomarker of Clinical Outcomes in Resectable Non-small Cell Lung Cancer.
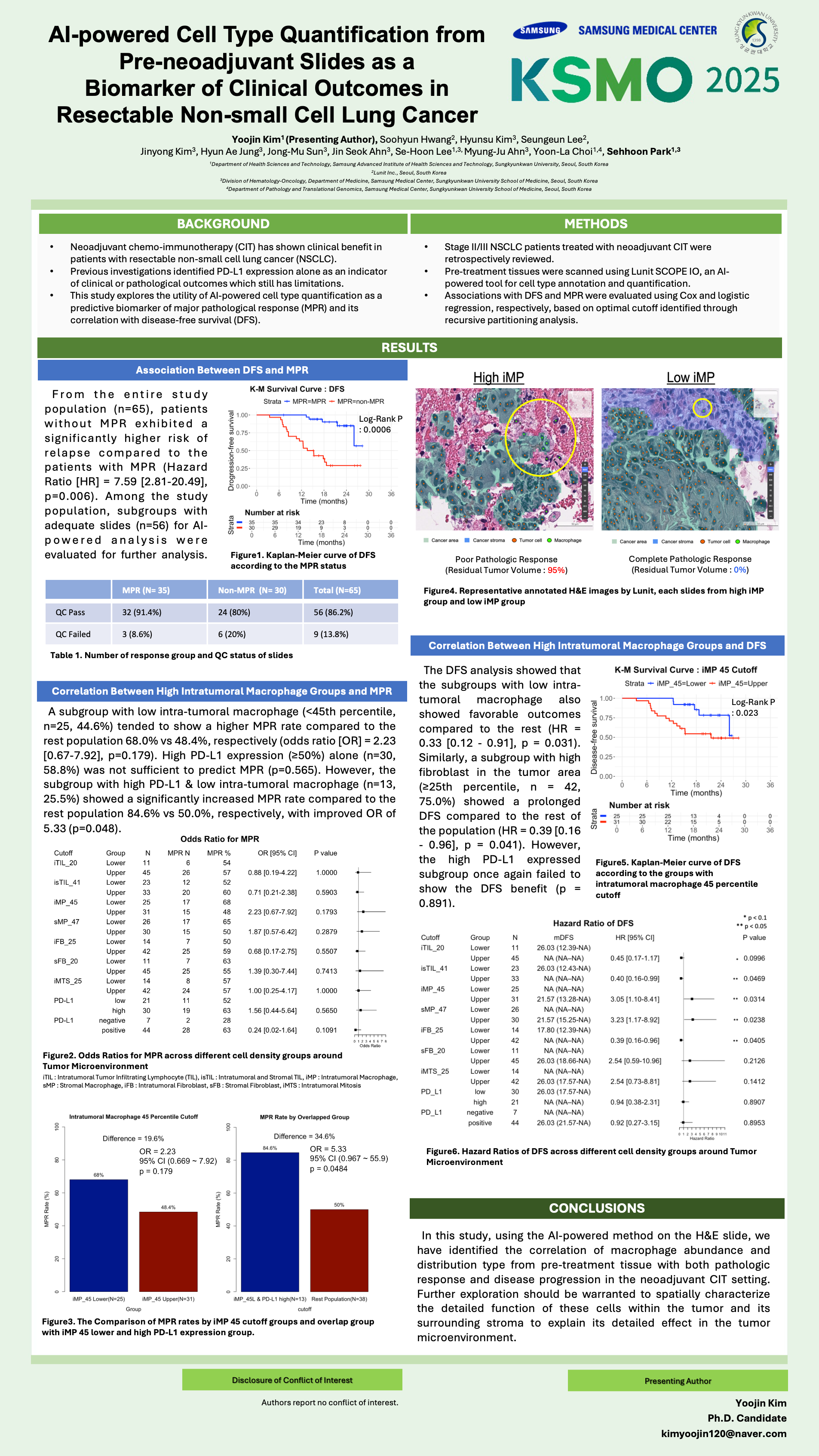
Background: Neoadjuvant chemo-immunotherapy (CIT) has shown clinical benefit in patients with resectable non-small cell lung cancer (NSCLC). Previous investigations identified PD-L1 expression alone as an indicator of clinical or pathological outcomes which still has limitations. This study explores the utility of AI-powered cell type quantification as a predictive biomarker of major pathological response (MPR) and its correlation with disease-free survival (DFS).
Methods: Stage II/III NSCLC patients treated with neoadjuvant CIT were retrospectively reviewed. Pre-treatment tissues were scanned using Lunit SCOPE IO, an AI-powered tool for cell type annotation and quantification. Associations with DFS and MPR were evaluated using Cox and logistic regression, respectively, based on optimal cutoff identified through recursive partitioning analysis.
Results: From the entire study population (n=65), patients without MPR exhibited a significantly higher risk of relapse compared to the patients with MPR (Hazard Ratio [HR] = 7.59 [2.81-20.49], p=0.006). Among the study population, subgroups with adequate slides (n=56) for AI-powered analysis were evaluated for further analysis. A subgroup with low intra-tumoral macrophage (<45th percentile, n=25, 44.6%) tended to show a higher MPR rate compared to the rest population 68.0% vs 48.4%, respectively (odds ratio [OR] = 2.23 [0.67-7.92], p=0.179). High PD-L1 expression (³50%) alone (n=30, 58.8%) was not sufficient to predict MPR (p=0.565). However, the subgroup with high PD-L1 & low intra-tumoral macrophage (n=13, 25.5%) showed a significantly increased MPR rate compared to the rest population 84.6% vs 50.0%, respectively, with improved OR of 5.33 (p=0.048). The DFS analysis showed that the subgroups with low intra-tumoral macrophage also showed favorable outcomes compared to the rest (HR = 0.33 [0.12-0.91], p=0.031). Similarly, a subgroup with high fibroblast in the tumor area (³25th percentile, n=42, 75.0%) showed a prolonged DFS compared to the rest of the population (HR = 0.39 [0.16-0.96], p=0.041). However, the high PD-L1 expressed subgroup once again failed to show the DFS benefit (p=0.891).
Conclusions: In this study, using the AI-powered method on the H&E slide, we have identified the correlation of macrophage abundance and distribution type from pre-treatment tissue with both pathologic response and disease progression in the neoadjuvant CIT setting. Further exploration should be warranted to spatially characterize the detailed function of these cells within the tumor and its surrounding stroma to explain its detailed effect in the tumor microenvironment.