KOGO 2026
Distinct Immune Crosstalk Axes Define the Tumor Microenvironment across EGFR Mutation Status in NSCLC by Single-Cell Profiling
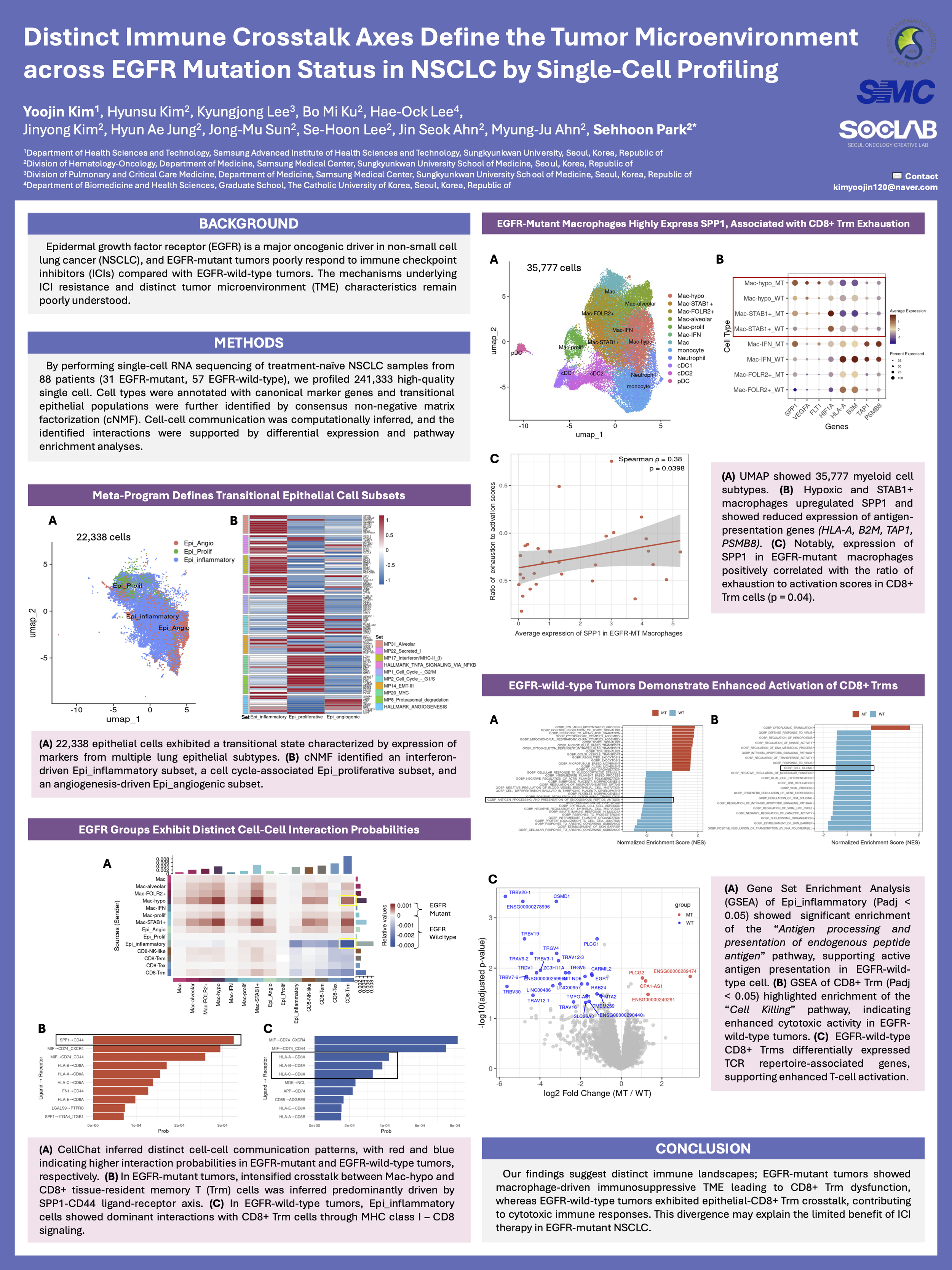
Background: Epidermal growth factor receptor (EGFR) is a major oncogenic driver in non-small cell lung cancer (NSCLC). Patients with EGFR-mutant NSCLC show limited responses to immune checkpoint inhibitors (ICIs) compared with those with EGFR-wild-type tumors, as previously reported. The mechanisms underlying primary ICI resistance and distinct tumor microenvironment (TME) characteristics in EGFR-mutant NSCLC remain poorly understood.
Methods: We performed single-cell RNA sequencing of treatment-naïve NSCLC samples from 88 patients (31 EGFR-mutant, 57 EGFR-wild-type) to characterize TME. Data processing, normalization, dimensional reduction, and clustering were conducted with Seurat package. Cell types were annotated with canonical marker genes, and transitional epithelial populations were further identified through consensus non-negative matrix factorization (cNMF). Cell-cell communication networks were computationally inferred, and the identified interactions were supported through differential expression and pathway enrichment analyses.
Results: By profiling 241,333 high-quality single cells, we identified 33,628 epithelial cells. cNMF revealed an inflammatory transitional epithelial (Epi_inflammatory) subset based on interferon-driven immune programs. In EGFR-wild-type tumors, these Epi_inflammatory cells showed dominant interactions with CD8+ tissue-resident memory T (Trm) cells through MHC class I–CD8 signaling. The epithelial cells exhibited higher expression of key antigen-presentation genes (B2M, TAP1, PSMB8/9), while CD8+ Trm cells showed elevated expression of cytotoxic markers (GZMB, PRF1, NKG7) and differentially expressed TCR repertoire-associated genes, indicating enhanced T-cell activation. GSEA showed enrichment of the “Cell killing” pathway in CD8+ Trm cells and “Antigen processing and presentation of endogenous peptide antigen” in epithelial cells, supporting dominant MHC class I-mediated interaction in EGFR-wild-type tumors.
In contrast, intensified crosstalk between tumor-associated macrophages (TAMs) and CD8+ Trm cells was inferred in EGFR-mutant tumors, predominantly driven by the SPP1-CD44 ligand-receptor axis. Hypoxic and STAB1+ TAMs displayed upregulated SPP1 levels and reduced antigen-presentation genes expression, while CD8+ Trm cells expressed higher CD44 levels. Notably, expression of SPP1 in macrophages positively correlated with the exhaustion score of CD8+ Trm cells (p = 0.041).
Conclusion: Our findings suggest distinct immune landscapes; EGFR-mutant tumors showed macrophage-driven immunosuppressive TME via SPP1-CD44 axis, leading to CD8+ Trm dysfunction, whereas EGFR-wild-type tumors exhibited epithelial-CD8+ Trm crosstalk, establishing a cytotoxic niche. This divergence may explain the limited benefit of ICI therapy in EGFR-mutant NSCLC.